Hair restoration is a highly sophisticated subspecialty that offers significant relief to patients with hair loss. An improved understanding of the aesthetics of hair loss and cosmetic hair restoration, hair anatomy and physiology, and the development of microvascular surgical instrumentation has revolutionized the approach to surgical hair restoration since the original description. Additional elements that contribute to the current state of the art in hair restoration include graft size, site creation, packing density, and medical control of hair loss. The results of hair restoration are natural in appearance and are provided with a very high level of patient satisfaction and safety. This aspect of cosmetic surgery is a very welcome addition to a traditional aesthetic practice and serves as a tremendous source for internal cross-referral. The future of hair restoration surgery is centered on minimal-incision surgery as well as cell-based therapies
Hair Restoration
Alopecia, the term for generic hair loss, involves a diminution of visible hair. There are numerous types of alopecia. The most common form of surgically treatable alopecia is androgenic alopecia (AGA). Throughout time, the presence of scalp hair has represented attributes of health, vigor, vitality, and strength. Accordingly, loss of hair in men (MAGA, or male pattern androgenic alopecia) and especially women (FPHL, or female pattern hair loss) can have significant psychosocial effects. The overwhelming majority of procedures for hair restoration are hair transplants, and the advent of microvascular surgical instrumentation as well as an improved understanding of the anatomy and physiology of hair loss has revolutionized the art of surgical hair restoration since the original description and early refinement
Anatomy, Genetics, and Physiology of Hair Loss
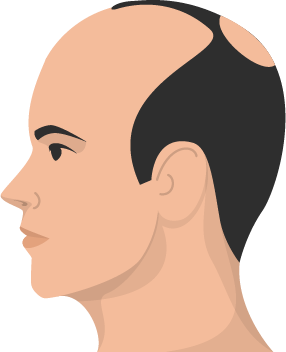
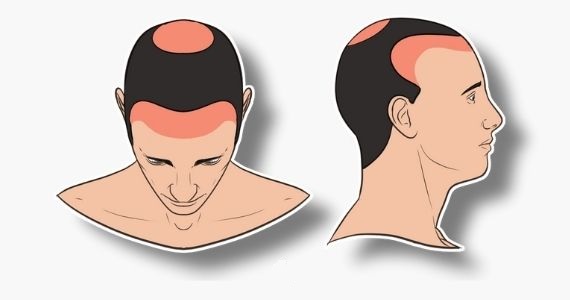
Androgenic alopecia is characterized by progressive visible thinning of scalp hair in genetically susceptible men and in some women. The current scientific data support the thesis that AGA is a polygenic trait. Significant associations have been reported with variant regions of the androgen receptor gene, which is located on the X chromosome. Epidemiologic surveys of AGA reveal the highest incidence in Caucasians, followed by Asians and then Africans, with the lowest incidence in Native American For the purpose of hair transplantation, the scalp may be divided into the frontal, midscalp, vertex, and temporal areas Hair thinning and subsequent shedding is due to gradual miniaturization of genetically marked hair follicles and represents shortening of the anagen (growth) phase of the hair follicle with an increase in the telogen/anagen ratio of the affected scalp. An understanding of the normal hair follicle life cycle is critically linked to an appreciation of the physiology of hair loss
In women, there is no consensus on whether hair loss is truly androgen dependent. Most women with FPHL do not have biochemical hyperandrogenism. In fact, some women without detectable circulating androgens may also develop FPHL, suggesting a possible role for non-androgen-dependent mechanisms. Based on this evidence, it seems appropriate to replace the term androgenic alopecia in women with the previously mentioned, more contemporary and scientifically descriptive term female pattern hair loss (FPHL), to include this recognized heterogeneity
Nonsurgical Options for Treating Hair Loss
General Evaluation
Young men and women are particularly distraught by the signs of hair loss. Low self-esteem and vulnerability to a fantasized outcome place this subset of patients at particular risk for quick decision making and unrealistic expectations. Managing these expectations and formulating a realistic surgical plan for patients with hair loss is a critical component to the long-term success of the procedure.
A fundamental concept that physicians and patients are advised to maintain during the evaluation and planning for HRS is that hair loss is progressive. The appearance of hair loss in the office during consultation is merely a snapshot along a continuum that began years earlier and will progress until death. Communication regarding the quality of the patient donor hair is also an additional essential component in managing expectations. The qualities of the hair that should be reviewed include curl, hair shaft diameter, color, texture, follicular unit density, and the telogen/anogen ratio of in situ donor hair. These aspects of the donor hair should be not only reviewed but also documented as a means to predict how well the transplanted hair will camouflage areas of scalp alopecia.
Hair Transplant Technique
As with any surgical procedure, the techniques of the operation will vary based on personal preference and clinical circumstances. Although the fundamental approach described herein is nearly universally applicable, the specific techniques do reflect most closely the methodology preferred by the lead author (JEV).
Anesthesia
Hair transplantation can be performed under local anesthesia alone or with supplemental sedation. The local anesthesia solution is a 40-mL mixture of 0.25% bupivacaine with 1:200 000 epinephrine + 20 mL 1.0% lidocaine with 1:200 000 epinephrine. This solution is used in the donor and recipient sites, and supplementation with additional bupivacaine 0.25% is performed in both regions of the scalp prior to discharge from the operating room. If conscious sedation is included with the procedure, the patient is premedicated with 1 to 2 mg PO aprazolam. In the operating room, an intravenous cocktail of ketamine 5 mg/mL, midazolam 0.5 mg/mL, and fentanyl 10 mcg/mL is titrated to achieve the desired level of sedation. All patients receiving any type of sedation are continuously monitored during the procedure with oximetry and receive supplemental nasal
Donor Site Harvest
In contemporary practice, follicular units can be obtained either through strip excision of the donor scalp with subsequent microscopic tissue dissection or by removal using a technique called follicular unit extraction (FUE)
Strip excision.
In preparation for the strip harvest, the selected area of donor hair is trimmed to 4- to 5-mm length and the patient is positioned in a lateral decubitus position. An ellipse of donor scalp is outlined, and following the administration of local anesthesia, tumescent saline solution is infiltrated. Tumescence in conjunction with precise knife blade angulation parallel to the hair shafts reduces follicle transection. Dissection level of the donor strip should be at the superficial fat to avoid injury to the occipital neurovascular bundle. The wound is closed in 2 layers, with an absorbable suture in the deep layer and a monofilament suture of choice at the level of the skin. Staples or dissolving sutures are also options
Follicular unit extraction.
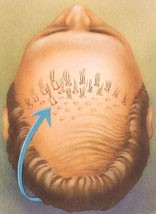
Follicular unit extraction is an alternative method of donor harvest. This technique is essentially a refined “micropunch grafting” version of the older punch graft technique. Using the current technique of FUE, 1 FU is removed at a time. There are several techniques and instruments to perform FUE. These include manual, power-assisted, and automated methods. No matter which technique is employed, the net result is still the isolation and removal of a single FU The remaining puncture is left to heal by secondary intention. Some hair transplant surgeons choose to employ FUE on a selective basis for small cases , whereas others select this donor harvest technique for their larger sessions The increased popularity of FUE has been linked to the development of power-assisted technology as well as a general trend toward minimally-invasive techniques. The indications, outcomes, and techniques for FUE as a donor harvest option are found elsewhere
Hairline Design and General Recipient Area
The first landmark that needs to be determined is the height of the anterior hairline (AHL) In most instances, the location of the most anterior, midfrontal portion of the hairline is between 7.5 and 9.5 cm above the glabella. The shape of the head, predicted future hair loss, and donor capacity are factors to consider in this creative decision. One must place the hairline in such a location that it will look natural as the patient matures and continues to lose hair.
If the temporal point is expected to recede, a higher hairline should be considered because a low hairline with a lost temporal point suggests a hairpiece. The temple point should be even or slightly posterior to the frontal hairline. Along with the aforementioned principles, a gently curving hairline should be created, with care taken to always maintain a significant frontal-temporal recession. Restoration of the temporal triangle is performed according to the personal preference of patient and surgeon.
The design should begin by ensuring the presence of a lateral hump . If the lateral hump is absent, this should be designed first. The lateral hump is the superior extension of the inferiorly directed hair of the temporoparietal fringe. The superior extent of this important landmark is even with or just medial to a line drawn vertically from the lateral canthus. This landmark is important because it represents the lateral extent of the AHL. The intersection of the lateral AHL and the lateral hump is the apex of the frontotemporal recession and should always be convex in a male AHL design
When a forelock pattern is created, the rear border should be located somewhere along the midscalp. Whether or not there is a plan to graft the vertex, the rear hairline should be constructed with an irregular border of small grafts. The lead author prefers to create a tapered posterior forelock pattern of trailing design that renders the crown less circular and mimics a natural variation on the balding process .A distribution of grafts recreating a natural whorl pattern can be constructed at the posterior aspect of the forelock. The crown area can be further grafted as indicated but should always be considered as an extension of the posterior forelock to maintain a natural distribution of hair
Conclusion of Procedure, Postoperative Care, and Emergence of Results
Hair transplants are lengthy procedures. A typical session of 1500 to 2500 grafts utilizing 4 assistants will last approximately 6 to 7 hours. The procedure is conducted using a clean technique with sterilized or disposable instruments. Postoperatively, the recipient sites and donor area are typically not bandaged, and perioperative antibiotics are not prescribed on a routine basis. Patient instructions include head elevation and icing of the forehead and donor area, along with analgesics. Aloe ointment administration to the grafted area and gentle shampooing in the shower should commence on postoperative day 2. Most of the recipient site eschars are gone by day 10, and donor sutures are removed on day 14. Although there are exceptions to the rule, most grafts enter a telogen phase for the first 3 months prior to entering their anagen phase. Full growth and evaluation of transplant results cannot reliably be assessed for 8 to 12 months following the procedure.